Neuropuncture: Redefining TBI and Migraine Management for Enhanced Well-Being
May 10, 2024We are excited to introduce our first-ever Neuropuncture workshop in Christchurch, dedicated to the advanced study of Traumatic Brain Injury and Migraine management through the innovative Neuropuncture system. This specialised workshop is designed to provide participants with a deep understanding of the pathophysiology, treatment, and recovery strategies for these challenging conditions.
Traumatic Brain Injuries and Migraines are not just prevalent health issues; they are intricate puzzles that require a nuanced understanding and a holistic approach to treatment. That's where Neuropuncture comes in, offering a unique blend of advanced needling techniques and electrical acupuncture with neuroscientific insights into the mechanism of these modalities related to TBI recovery. At our upcoming workshop in Christchurch participants will learn about crucial topics such as:
- The intricate pathophysiology of Traumatic Brain Injury and its effects on the body and mind.
- The role of Autonomic Nervous System Dysregulation in TBI and its implications for recovery.
- The critical impact of Neuroinflammation on brain health and how to address it.
- The significance of Gut Dysbiosis in the recovery process from TBI.
- Techniques for addressing Visual and Vestibular Mismatch in TBI patients.
- The importance of considering Cervical Spine issues in TBI management.
- The overlap between psychological factors and TBI recovery.
- A comprehensive exploration of Migraines, including different types and their unique challenges.
- Special considerations for ocular Migraines and how to approach them.
Whether you're an experienced practitioner or new to the field of Neuropuncture, this workshop in Christchurch will equip you with the knowledge, skills, and insights needed to make a real difference in the lives of those suffering from these debilitating conditions.
Let's take a quick dive into some of the content we will be covering at the workshop:

Exploring the Trajectory of Chinese Medicine Traumatology
Woven into the intricate fabric of Chinese medicine, one finds a rich tapestry with ancient insights, practices, and texts that have profoundly shaped the discipline across millennia. This blog post traces the evolution of Chinese medicine traumatology from its beginnings to its pivotal role in contemporary medical practice.
The Genesis of Traumatology in Chinese Medicine
The genesis of Chinese medicine traumatology can be traced back to ancient texts (such as the "Rites of Zhou") dedicated to wound management. Dating back to the Zhou Dynasty, this historical record mentions specialised government physicians adept in the treatment of cutaneous and muscular injuries, showcasing an early systematisation of trauma care in ancient China.
Unveiling Medical Treasures at Mawangdui Tombs
The unearthing of medical manuscripts within the Mawangdui tombs, sealed in 168 BCE, heralded a pivotal moment in understanding ancient Chinese traumatology. These parchments unveiled sophisticated methodologies for addressing lacerations, illuminating the advanced medical practices prevalent during that era.
Ancient Modalities and Remedies
Early practitioners of Chinese traumatology employed a myriad of therapeutic modalities for managing injuries, encompassing herbal formulations, manual manipulations, movement and breath therapies and the venerable art of acupuncture. Anchored in the holistic precepts of Chinese medicine, these modalities sought to rehabilitate traumatic injuries from both a physical, mental and sprirtual perspective, fostering bespoke healing tailored to the individual.
The Evolution of Trauma Care in Chinese Medicine
During the Qing dynasty, Chinese medical scholars codified centuries of accumulated wisdom into systematic frameworks describing various categories of injuries. These classifications, as documented in texts such as "Yi Lin Gai Cuo" (Correcting Errors in Medical Classics) and "Wai Ke Zheng Zong" (Orthodox Canon of External Medicine) compiled by Wu Qian, spanned from initial wound management to the nuanced treatment of complex traumas encompassing wound debridement, fracture reduction, and analgesia strategies. Additionally, these treatises addressed surgical interventions, hemorrhage control, and methodologies to expedite wound healing and mitigate infection.
Acupuncture: An Integral Therapeutic Modality
In Chinese medicine traumatology, acupuncture stands as a fundamental therapeutic modality deeply ingrained in ancient healing practices. Its historical application spans millennia, demonstrating efficacy in pain alleviation, inflammation reduction, and promotion of innate healing mechanisms.
Acupuncture, a cornerstone of traditional Chinese medicine (TCM), serves as a versatile intervention in trauma management. Historically, distinct types of acupuncture needles were utilized to target varied aspects of traumatic injuries. Traditional slender and filiform needles aimed at specific neural vascular nodes, fostering pain relief and inflammation reduction through gentle insertion and manipulation.

Beyond needling techniques, specialized approaches augment acupuncture's role in trauma care. Tuina, a therapeutic massage modality, synergizes with acupuncture by rectifying connective tissue dysfunction, joint realignment, and neural vascular node stimulation, fostering musculoskeletal recovery. Herbal liniments, topically applied, further enhance healing by alleviating pain, reducing inflammation, and improving circulation, particularly potent when used post-acupuncture intervention.
Cupping therapy, often coupled with acupuncture, bolsters trauma treatment by enhancing blood flow, toxin elimination, and muscle tension relief, benefiting soft tissue injuries. Moxibustion, employing burnt mugwort as a heating thermal stimulus to improve circulation, complements acupuncture, especially in addressing trauma-related pain and stiffness.
Through a diverse toolkit, practitioners customize interventions to individual patient needs, addressing not only physical trauma but also emotional and psychological facets, fostering holistic healing. The amalgamation of ancient wisdom with contemporary innovations, notably within acupuncture, holds promise for advancing trauma care, respecting the intricate resilience and recuperative potential of the human body.
The early development of electro-acupuncture saw pivotal moments in the mid-20th century, notably in China during the 1930s and gaining momentum in the 1950s. In these formative years, pioneering researchers and practitioners began experimenting with the integration of electrical stimulation into acupuncture therapy, spurred by a confluence of traditional Chinese medical theories and burgeoning insights from Western neurology.
One influential figure in this early development was Dr. Han Jian, a Chinese physician renowned for his contributions to acupuncture research. In the 1930s, Dr. Han conducted groundbreaking experiments involving electrical stimulation applied to acupuncture needles. These experiments laid the groundwork for the utilization of electrical currents in acupuncture practice, opening new avenues for exploration and innovation.
The 1950s marked a turning point when researchers, inspired by Dr. Han's work, began systematically investigating the therapeutic potential of electro-acupuncture. This period witnessed the emergence of clinical studies aimed at elucidating the mechanisms underlying electro-acupuncture's effects on pain relief, inflammation reduction, and overall healing processes.
Among the notable early researchers was Dr. Cheng Dan'an, a neurophysiologist whose pioneering studies provided valuable insights into the neural mechanisms involved in acupuncture and electro-acupuncture. Dr. Cheng's work shed light on how electrical stimulation applied to acupuncture points modulates neural pathways, influencing pain perception and regulatory mechanisms within the central nervous system.

These early investigations laid the foundation for the integration of electro-acupuncture into clinical practice, paving the way for its widespread adoption and further refinement in subsequent decades. The pioneering efforts of researchers like Dr. Han Jian and Dr. Cheng Dan'an played a crucial role in establishing electro-acupuncture as a distinct therapeutic modality within the broader framework of traditional Chinese medicine.
Their work not only expanded our understanding of acupuncture's mechanisms of action but also catalyzed a paradigm shift in the application of electrical stimulation for therapeutic purposes. This early development phase set the stage for the evolution of electro-acupuncture into Neuropuncture, a modern approach that integrates traditional acupuncture principles with contemporary neuroscientific insights to optimize trauma care and promote holistic healing.
Understanding the Impact
of
Traumatic Brain Injuries
in
New Zealand:
A Closer Look at Concussion Statistics

In New Zealand, the issue of traumatic brain injuries (TBIs) is more prevalent than many might assume, affecting a significant portion of the population each year. With an estimated 35,000 individuals suffering from TBIs annually, the scale of this health concern is substantial. However, what is even more alarming is the treatment gap that exists, with a considerable number of those affected not receiving the necessary medical evaluation and care.
The Prevalence and Severity of TBI
Of the estimated 35,000 TBIs reported annually in New Zealand, a staggering 95% (equivalent to 33,250 individuals) are classified as mild traumatic brain injuries (mTBIs). Despite the classification as "mild," the potential long-term effects of these injuries should not be underestimated, as they can lead to significant health issues if left untreated. Yet, the current treatment statistics reveal a concerning trend: only around 22,000 of these cases are treated by health providers each year. This discrepancy highlights a critical gap in healthcare access or awareness, leaving a majority of those affected without professional medical assessment or intervention.
The Leading Causes of TBIs
Understanding the primary causes of TBIs in New Zealand is crucial for developing targeted prevention and treatment strategies. The leading causes include:
1. Falls: These incidents represent a significant proportion of TBIs, affecting individuals across all age groups. Falls can occur in various settings, from the home to outdoor environments, and can result in injuries ranging from mild to severe.
2. Recreation and Sports: Engaging in recreational activities and sports accounts for 20% to 30% of TBIs. While physical activity is essential for health and well-being, it also poses risks, particularly in contact sports or activities involving high speeds or heights.
3. Machinery Use: Operating machinery, whether in industrial settings or during DIY projects at home, can lead to accidents resulting in TBIs. Proper safety measures and training are crucial to minimizing these risks.
4. Driving Accidents: Road traffic accidents are a significant source of TBIs, underscoring the importance of road safety measures, responsible driving, and the use of protective gear such as helmets.
5. Assault: Unfortunately, assaults are also a cause of TBIs in some cases, highlighting broader social and safety issues that need to be addressed.
Bridging the Treatment Gap
The gap between the number of TBIs occurring each year and the number of those receiving treatment is a pressing concern. It underscores the need for increased awareness about the importance of seeking medical attention after any head injury, no matter how minor it may seem. Public health campaigns, education on the symptoms of TBIs, and improved access to healthcare services are essential steps in ensuring that more New Zealanders receive the care they need.
Moving Forward
Addressing the challenge of TBIs in New Zealand requires a multifaceted approach, involving healthcare providers, policymakers, community organizations, and individuals. By increasing awareness, improving access to care, and implementing preventive measures, it is possible to reduce the incidence of TBIs and ensure that those affected receive timely and effective treatment. As a society, recognizing the seriousness of TBIs and taking proactive steps to address this issue is crucial for the health and well-being of all New Zealanders.
Exploring the Frontiers of Neuropuncture in Traumatic Brain Injury Research
In the realm of traumatic brain injury (TBI) treatment, Neuropuncture stands as a beacon of innovation, merging ancient healing practices with modern neuroscientific research. This cutting-edge approach investigates the complex pathophysiological components of TBI, aiming to unravel and address the underlying mechanisms through targeted research and clinical applications. Let's look into three pivotal areas of investigation that highlight the potential of Neuropuncture in transforming TBI care.
1. Gut-Brain Axis Neuro-regulation
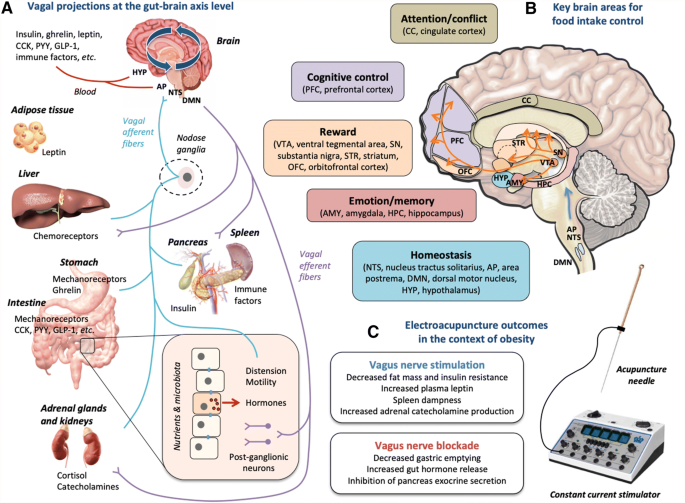
One of the most intriguing aspects of TBI research within the scope of Neuropuncture is the exploration of the gut-brain axis and its neuro-regulation. TBI can disrupt the corticopontine connections, affecting the vagus complex and leading to dysautonomia. This disturbance significantly impacts the brain-gut axis, potentially resulting in physiological intestinal changes and alterations in the gut microbiome. Moreover, TBI is associated with increased intestinal permeability, attributed to the decreased expression of intestinal tight junction proteins such as ZO-1 and occludin. This disruption can lead to systemic inflammation, bacterial translocation, and even sepsis. Neuropuncture's targeted interventions aim to restore the delicate balance of the gut-brain axis though Vagus nerve stimulation, offering a promising avenue for mitigating these TBI-induced complications.
2. Rehabilitating Damaged Brain Tissue
The potential of Neuropuncture to facilitate the rehabilitation of damaged brain tissue is another area of significant research interest. This approach focuses on promoting cell proliferation within the central nervous system, particularly in neurogenic areas and certain ischemic tissues. Neuropuncture techniques are being explored for their ability to regulate cerebral blood flow through angiogenesis and the modulation of vasoactive mediators. Additionally, these techniques offer anti-apoptotic benefits, intervening in the intrinsic and extrinsic pathways or related pathways that are crucial for brain tissue recovery. Neuropuncture's regulation of neurochemicals involved in neurotransmission, antioxidants, inflammatory substances, neurotrophic factors, and metabolic substrates further underscores the comprehensive potential of Neuropuncture in TBI treatment. 
3. Regulating Brain Network Connectivity
The modulation of brain network connectivity, particularly within the Default Mode Network (DMN), represents a groundbreaking area of Neuropuncture research in TBI. Brain regions within the DMN overlap significantly with acupuncture-responsive regions, suggesting that acupuncture can modulate the DMN's functionality. This modulation includes both local activation/deactivation and alterations in the functional connectivity within and across the DMN. Notably, acupuncture-induced regulation of the DMN is more pronounced than that achieved through sham acupuncture or tactile stimulation, with the effects being attenuated or reversed if sharp pain occurs during the procedure. Furthermore, increasing the "dose" of acupuncture—by augmenting the number of needles or the intensity of needle stimulation—may enhance the modulation within the DMN, with effects persisting even after the cessation of acupuncture stimulation.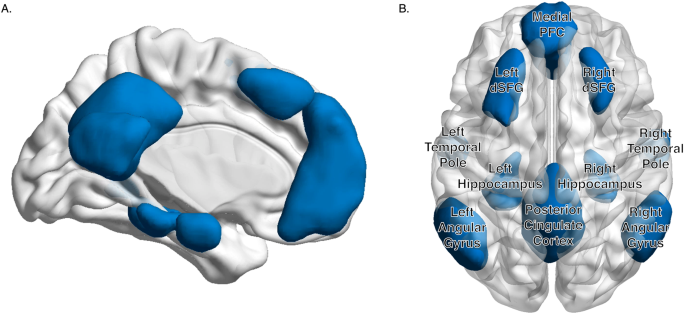
As we continue to explore the vast potential of Neuropuncture in the context of traumatic brain injury, these three areas of research offer a glimpse into the future of TBI treatment. By addressing the gut-brain axis, rehabilitating damaged brain tissue, and regulating brain network connectivity, Neuropuncture paves the way for innovative, holistic approaches to healing and recovery. The journey of integrating ancient wisdom with modern science continues, promising new horizons in the care and treatment of TBI patients.
Migraines
Unraveling the Connection: Migraines and Traumatic Brain Injury
Migraines and traumatic brain injury (TBI) share a complex and intertwined relationship, with TBI often acting as a catalyst for triggering or exacerbating migraine headaches. This intricate connection goes beyond mere coincidence reviling a multifaceted pathophysiology that intertwines the aftermath of physical trauma with the neurological intricacies of migraine episodes. In this section of the blog, we aim to shed light on the key aspects of how traumatic brain injuries can influence and precipitate migraine headaches, offering insights into their interconnected pathophysiology.
Key Points in the Pathophysiology of Migraines Related to TBI
1. Neuroinflammation: One of the primary responses to traumatic brain injury is neuroinflammation. This inflammatory response, while part of the body's attempt to repair and protect the brain, can also lead to increased sensitivity and susceptibility to migraine headaches. The release of pro-inflammatory cytokines and other inflammatory mediators can exacerbate migraine pathophysiology, making the brain more prone to migraine attacks.
2. Disruption of the Blood-Brain Barrier (BBB):TBI can compromise the integrity of the blood-brain barrier, a critical defense mechanism that protects the brain from harmful substances. When the BBB is disrupted, it allows potentially neurotoxic substances to enter the brain's environment, which can contribute to the development or worsening of migraine headaches.
3. Neuronal and Axonal Damage: The physical impact of TBI can cause direct damage to neurons and axons, leading to a cascade of neurochemical changes that affect brain function. This damage can alter the way the brain processes pain signals, increasing the likelihood of migraine episodes. Additionally, the repair and regeneration processes following neuronal damage can further alter neuronal excitability and sensitivity, contributing to migraine pathophysiology.
4. Alterations in Neurotransmitter Levels: Traumatic brain injury can lead to imbalances in various neurotransmitters, including serotonin, dopamine, and glutamate, which play crucial roles in the regulation of pain and mood. These imbalances can contribute to the heightened pain perception and emotional disturbances often associated with migraines.
5. Cervical Injury and Muscle Tension: TBI is frequently accompanied by cervical injuries or increased muscle tension in the neck and head region. This physical strain can act as a trigger for migraine headaches, as it affects the nerves and blood vessels that are already sensitized due to the injury.
Exploring the Diverse Faces of Migraine:
A Journey into Its Subcategories
Migraine, often termed a "silent epidemic," profoundly impacts millions globally, with its diverse presentations posing unique challenges. Despite its common perception as a singular entity, migraine manifests in various subcategories, each characterized by distinct features and underlying mechanisms. Let's delve deeper into these subtypes:
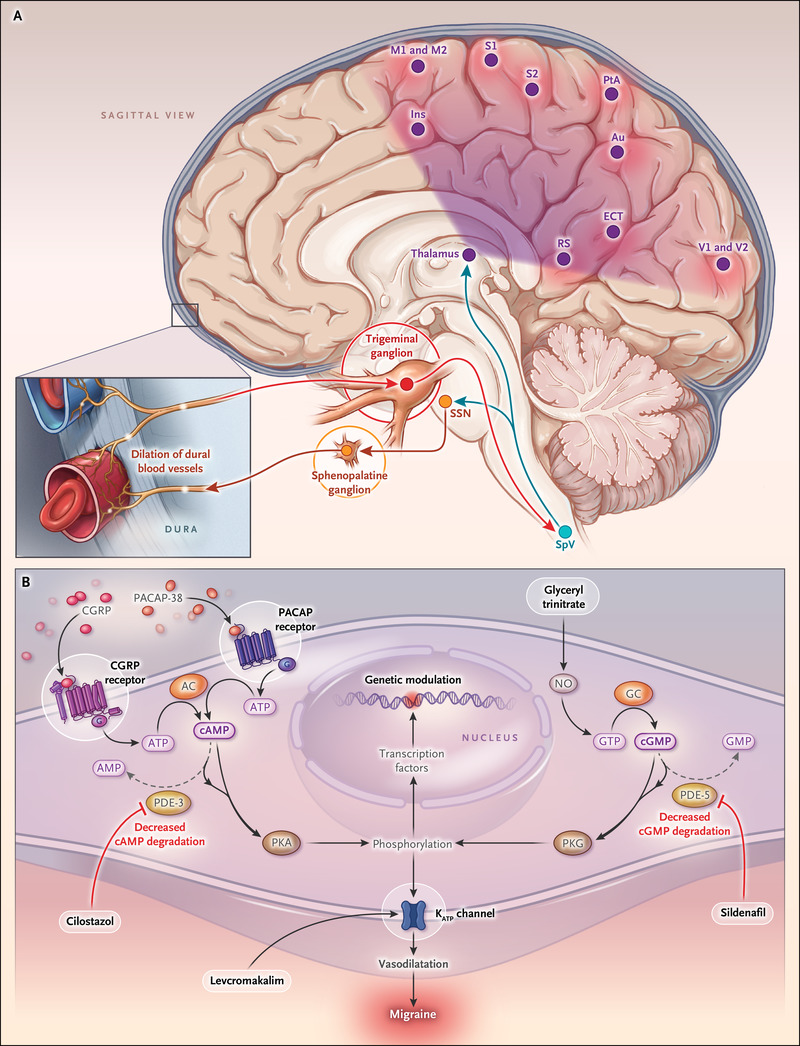
1. Migraine with Aura: A Multifaceted Neurological Phenomenon
Migraine with aura presents an intriguing array of sensory disturbances preceding headaches. These manifestations, ranging from visual flickers to sensory changes, offer glimpses into cortical spreading depression (CSD), a wave of neuronal activity alteration. CSD, believed to originate from the brain's occipital and somatosensory regions, sheds light on migraine's pathophysiology, emphasizing the intricate interplay between cortical excitability and trigeminal nociception.
2. Migraine without Aura: Unraveling the Essence of Pain
Devoid of aura, migraine without aura manifests as intense headaches accompanied by nausea and sensitivity to stimuli. While its exact etiology remains enigmatic, neurovascular dysregulation and trigeminovascular system activation are pivotal. Cortical hyperexcitability and disrupted pain modulation pathways contribute to migraine genesis, exacerbated by alterations in neurotransmitter levels such as serotonin and CGRP.
3. Chronic vs. Episodic Migraine: Navigating Frequency Dynamics
Chronic migraine engulfs daily life, contrasting episodic migraine's intermittent pain episodes. The transition from episodic to chronic migraine entails intricate neurobiological alterations, including aberrant pain processing and cortical sensitization. Dysfunctional pain modulation pathways and maladaptive neuroplasticity perpetuate migraine attacks, underscoring the significance of timely intervention and tailored management strategies.
4. Menstrual Migraine: Hormonal Influences on Migraine Dynamics
Menstrual migraine synchronizes with hormonal fluctuations, particularly estrogen withdrawal preceding menstruation. Hormonal variations modulate cortical excitability, neurotransmitter release, and neurovascular coupling, influencing migraine susceptibility across the menstrual cycle. Understanding the intricate hormonal-brain interplay is crucial for optimizing therapeutic interventions and alleviating the burden of menstrual migraine.
5. Basilar-Type Migraine: Unveiling Brainstem Dysfunction
Basilar-type migraine unveils a spectrum of symptoms, including vertigo and visual disturbances, implicating brainstem nuclei dysfunction. Disrupted neurotransmitter signaling, particularly involving serotonin and GABA, contributes to aberrant neuronal activity and cortical spreading depression. Unraveling brainstem dysfunction promises targeted therapeutic approaches for enhanced patient outcomes.
6. Hemiplegic Migraine: Traversing Neurological Territory
Hemiplegic migraine manifests as transient paralysis and sensory disruptions, associated with genetic mutations affecting ion channels and neurotransmitter receptors. Cortical spreading depression across brain hemispheres underscores cortical hyperexcitability's pivotal role in hemiplegic migraine pathogenesis. Deciphering molecular mechanisms offers insights into broader neurobiological pathways implicated in migraine and related disorders.
7. Retinal Migraine: Insight into Visual Vulnerability
Retinal migraine presents reversible monocular visual disturbances, intertwined with retinal vasculature dysfunction and neurovascular dysregulation. Vasospasm of retinal arteries induces transient ischemia, precipitating visual dysfunction preceding or accompanying migraine attacks. Understanding retinal migraine's multifaceted nature elucidates its implications for visual health and therapeutic interventions.
In navigating migraine subtypes, we unravel the intricate interplay between genetic predisposition, environmental triggers, and neurobiological mechanisms. By discerning each subtype's unique features, we pave the way for personalized approaches to diagnosis, treatment, and management, fostering optimal care and support for every migraineur. Join us on this enlightening journey as we deepen our understanding of migraine complexities and embark on pathways toward tailored care and patient empowerment.
Neuropuncture's Role in Migraine Care
Understanding the Neurobiological Terrain:
At the forefront of Neuropuncture's migraine protocol lies a profound understanding of the neurobiological terrain of migraines. From the intricate interplay of neurotransmitters to the dysregulation of pain processing pathways, every facet of migraine pathophysiology becomes a potential target for intervention. Neuropuncture practitioners investigate the neural substrates of pain perception, inflammation, and neuroendocrine regulation, forging a nuanced understanding of the interconnected mechanisms at play.
Navigating Neuropuncture's Therapeutic Landscape:
The essence of Neuropuncture's approach lies in its ability to modulate the intricate bioelectric circuits woven throughout the nervous system. By harnessing the power of electrical stimulation, Neuropuncture practitioners navigate the neural pathways implicated in migraine pathogenesis, offering targeted neuromodulation to alleviate pain, reduce inflammation in the trigeminal vascular network, and restore neural homeostasis, Neuropuncture offers a multifaceted approach to migraine care.
Pioneering a Path Forward:
In the landscape of migraine treatment, Neuropuncture heralds a paradigm shift that brings hope and tangible relief to sufferers. As neuroscience, acupuncture, and bioelectronics converge at the forefront of migraine care, Neuropuncture emerges as an innovator offering a promise of a more pain-free and balanced life becomes increasingly within reach for migraine sufferers, marking a transformative leap toward improved quality of life and well-being.
We invite you to join us in Christchurch for our upcoming workshop on TBI and migraines, where we will gain insight into the Neuropuncture approach to treatment. This is a unique opportunity to learn from experts in the field, gain practical hands on training in advanced needling techniques and functional assessment skills, and connect with others who share your interest in advancing the care and treatment of these complex conditions. Together, we can pave the way for advancements in the management of migraines and traumatic brain injuries. Don't miss this chance to be part of a pioneering community dedicated to making a real difference in the lives of those affected.
Join us in Christchurch and be a part of this transformative journey.
Register here:

Pete Larking
Medical director of Neuromedtec
Neuropuncture Instructor
Join us at the Stillness in Motion 5 hour retreat May 17th in Wairarapa
Limited spaces available so secure your spot today!
